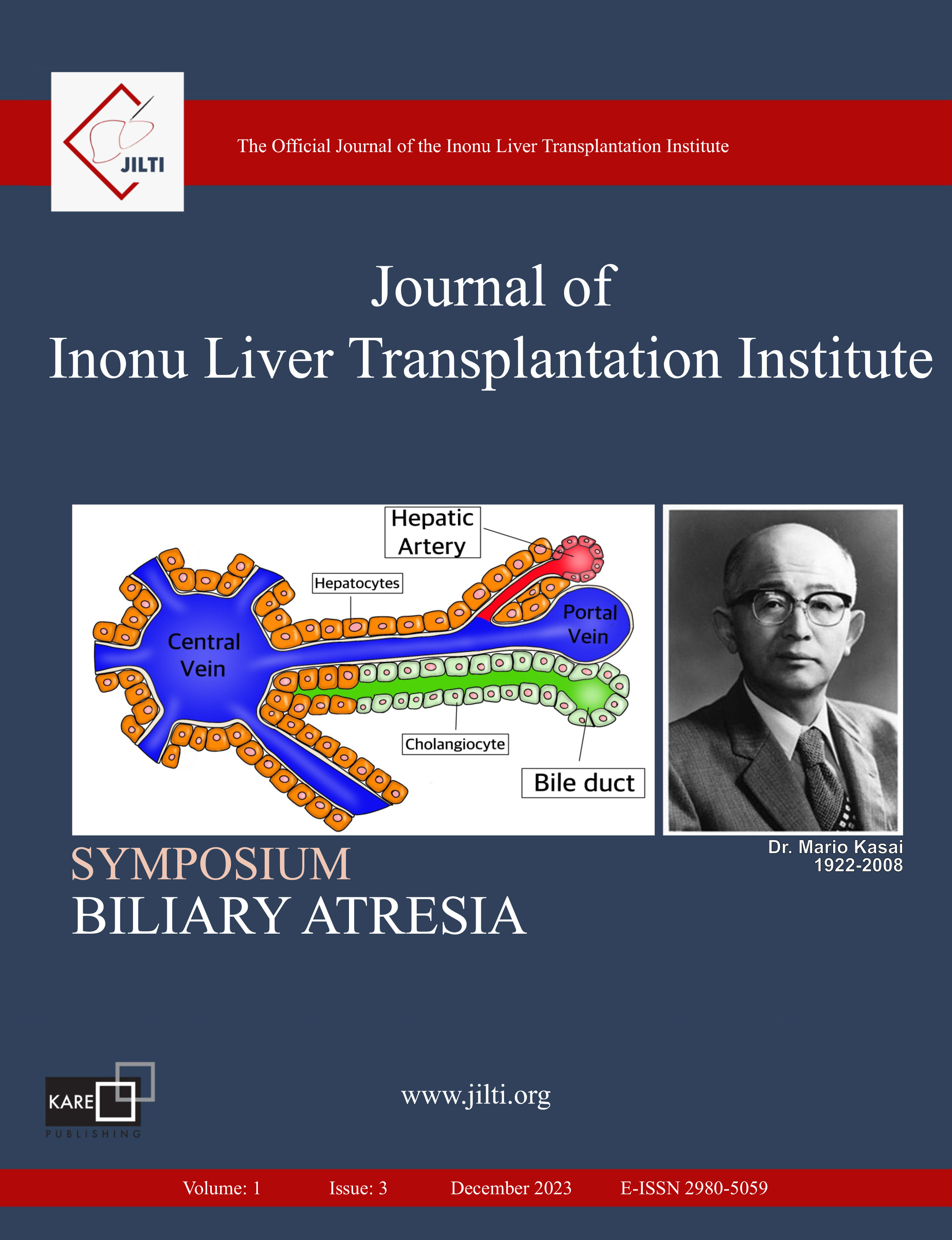
Evaluation of a Case with Biliary Atresia and Heterotaxy Syndrome (Left Isomerism) in Terms of Liver Transplantation: A Case Report
Huseyin Ayvaz, Sevgi Demiroz TasolarDepartment of Pediatric Radiology, Department of Radiology, Faculty of Medicine, Inonu University, Malatya, TürkiyeLeft isomerism, a subtype of heterotaxy marked by multiple spleens and abnormal organ positioning, poses additional complexity when coexisting with biliary atresia, the leading cause of neonatal cholestasis and pediatric liver transplantation. We report a 5-month-old male infant with biliary atresia and left isomerism, presenting with persistent jaundice, acholic stools, and dark urine. Despite undergoing Kasai portoenterostomy at one month, clinical and laboratory parameters did not improve. Cardiac assessment revealed left atrial isomerism, atrioventricular septal defect, pulmonary atresia, and patent ductus arteriosus. Abdominal CT showed a midline liver, polysplenia, absent inferior vena cava with azygos-hemiazygos continuation, preduodenal portal vein, intestinal malrotation, and visceral heterotaxy. Laboratory tests indicated severe cholestasis, hepatocellular injury, and impaired liver function. The patient was evaluated and listed as a liver transplant candidate. The coexistence of biliary atresia and left isomerism complicates both diagnosis and treatment. Early imaging, multidisciplinary management, and timely transplantation are essential to improve outcomes. This case underscores the importance of a comprehensive, individualized approach in managing biliary atresia with complex congenital anomalies.
Keywords: Biliary Atresia, Heterotaxy Syndrome, Liver Transplantation
Manuscript Language: English